

As Veteran’s Day approaches, we wanted to share some supportive information for those who care about the wellness of our military members, our Veterans, former and current military spouses, and friends and families of those who volunteer to defend the United States. We’re honored to be a Veteran Ready organization that was recognized by Governor Evers for our onboarding program that supports and empowers those who sacrifice so much for us all.
Transitioning from military service to civilian life can be a challenging process that often brings about a variety of mental health issues. Some of the most common challenges include:
1. Adjustment Disorder: The shift from a highly structured military environment to the more flexible civilian world can lead to adjustment disorders, characterized by stress, anxiety, and depressive symptoms as individuals adapt to new roles and routines.
2. Post-Traumatic Stress Disorder (PTSD): Veterans may continue to struggle with PTSD from combat or other traumatic experiences during their service, affecting their ability to integrate into civilian life.
3. Depression: The loss of camaraderie, identity, and sense of purpose associated with military service can contribute to feelings of sadness, hopelessness, and depression.
4. Anxiety: Uncertainty about employment, financial stability, and fitting into civilian society can lead to heightened anxiety levels.
5. Substance Abuse: Some Veterans may turn to alcohol or drugs as a coping mechanism for dealing with stress, trauma, and the difficulties of reintegration.
6. Identity and Purpose Issues: The transition often involves a significant change in identity and a loss of the sense of purpose and belonging that military service provides, leading to existential questions and a struggle to find new meaning in civilian life.
7. Relationship Strain: Reintegration can put a strain on family relationships and friendships, as Veterans and their loved ones adjust to changes in roles and dynamics.
8. Occupational Challenges: Finding and adjusting to civilian employment can be difficult, leading to frustration, low self-esteem, and financial stress. Veterans may also struggle to translate their military skills and experience into civilian job qualifications.
9. Social Isolation: Veterans may feel isolated due to a perceived lack of understanding and support from the civilian community, leading to loneliness and social withdrawal.
10. Moral Injury: Experiences that conflict with one’s moral or ethical beliefs can result in moral injury, causing profound guilt, shame, and spiritual distress.
11. Crisis: The combination of these mental health challenges can lead to crisis, particularly if Veterans feel overwhelmed or lack adequate support.
12. Healthcare Navigation: Navigating the civilian healthcare system to access mental health services and benefits can be confusing and frustrating, further exacerbating stress and mental health issues.
Addressing these challenges often requires a comprehensive support system, including access to mental health services, peer support groups, employment assistance programs, and community resources specifically designed for veterans transitioning to civilian life.
#veterans#VeteransDay2024#VeteransDay#veteranready#veteransupport

October is National Bullying Prevention Month and in this week’s episode of “Awkward Conversations,” an encore from Season 3, Jodie Sweetin of “Full House” and “Fuller House” and clinical psychologist Dr. Krystal Lewis are joined by anti-bullying advocate and author Jodee Blanco. Together, they dive into the emotional toll of bullying and how it can lead to substance use.
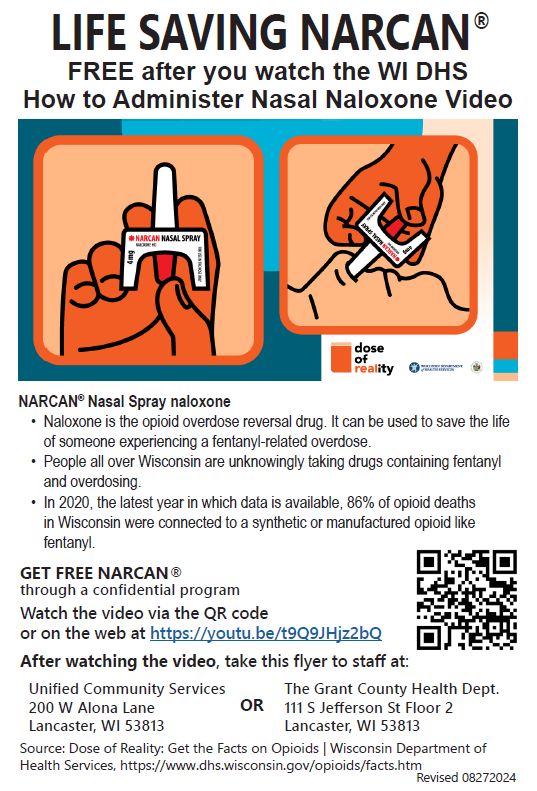

For those who may be at high-risk for an opioid overdose, you can have naloxone discretely mailed to you at no cost. See the link below.
Free fentanyl test strips are available by mail to residents of Wisconsin. Test strips are an excellent tool but need to be part of an overall harm reduction strategy. Also see the link below.